- General Information
- Health
- Society
- Media
- Become a MemberPREMIUM
- Events
- Contact Us
- Shop
- Categories
- Access to Health
- Ageing & Longevity
- Asset-Based Community Development
- Community & Health
- Ecology & Environment
- Economic & Political Root Causes
- Economic Stability
- Education
- Environmental Contaminants
- Ethnicity & Gender
- Health Condition of the Body
- Holistic Approach
- Law & Human Rights
- Men’s Health
- Natural Medicine
- Nutrition & Food
- On A Philosophical & Ethical Note
- Political Acceptance & Opposition
- Race
- Social Determinants of Health
- Traditional Medicine & Adjuvant Therapies
- Transhumanism
- Wellness
- Women’s Health
CHOLESTEROL AND STATINS: A MYTH IN NEED OF A REALITY CHECK? AN INDUCTIVE PARADIGM CHALLENGE!
A myriad of non-aligning findings….where is the logic?
The controversy on cholesterol and statins is coming to a boiling point. While most medical schools still train students within the cholesterol paradigm, and statins are considered and promoted as the primary solution, science has evolved significantly over the last two decades. Maybe it’s time to bury the hatchet and search for the real root causes of atherosclerosis, cardiovascular diseases (CVDs), and related comorbidities and mortality.
WHAT’S THE ORIGIN OF THE CHOLESTEROL PARADIGM?
If you talk to a doctor about this, most are completely unaware of how the cholesterol story unfolded in the 1950s. Dr. Ancel Keys was an influential and prominent researcher in the 1950s, convinced of a direct association between saturated fats and heart disease, although he had little causal evidence. He stated openly and loudly that people in the Mediterranean were healthier because they consumed less saturated fats, and it became his single point of focus. He was eager to prove a direct link between the two. In 1955, he presented a paper at the WHO called ‘The Six Countries Study’, which was later changed to ‘The Seven Countries Study’ as he initially failed to convince the WHO. Nonetheless, Keys presented his updated study, but the methodological design was very weak. His design, based on aggregated data as units of research, instead of using individual data, is not suitable for valid inferences, consequently leading to an ‘ecological fallacy’. Simply stated, Keys was making assumptions about individual people based on trends seen in a group. As if stating that in an affluent city, everyone must be rich, while only a few percent are responsible for the higher average income, and most people are average earners.
Meanwhile, in the UK, a British doctor, John Yudkin, argued carbs were the real culprit of cardiovascular disease development. However, Keys succeeded in selling his Seven Countries Study to a broad audience of politicians and influential people; some researchers state he deliberately used the fallacy model to make his point (Sinatra et al. 2014). Some still argue today that Keys published a seminal paper that should be considered as a milestone in preventing heart disease (Aboul-Enein et al. 2020). Keys tried to establish an association between dietary lipid uptake and high cholesterol levels, but failed to prove a direct link. Implementing different fat-based diets (cholesterol, saturated fats, Monounsaturated Fats (MUFA), Polyunsaturated Fats (PUFA,…) in different settings remained inconclusive. The Seven Countries study wasn’t covering the countries as a whole; only some local communities were investigated (selection bias).
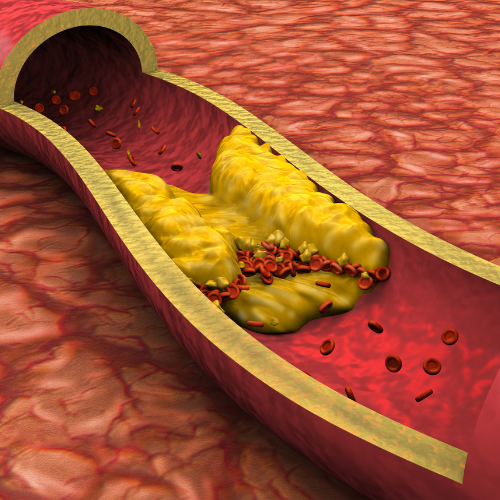
The methodology was inherently observational, which does not allow for proving any causation. Nonetheless, Keys presented his follow-up data at the WHO and concluded that fatty foods contributed to the development of atherosclerosis (plaque in the arteries), which was purported as the key driver for cardiovascular disease. The follow-up studies in the next decades couldn’t prove a causation between a fat-rich diet and CVDs; however, cholesterol showed a positive correlation with heart disease. Other factors that could have contributed were not investigated or left out of the equation. Only sucrose was studied by Keys, leaving out all the other carbs, and even with sucrose, Keys found a strong positive association, but remained convinced that only ‘bad fats’ (LDL-Cholesterol, saturated fats,…) were the cause of cardiovascular issues (Sinatra et al. 2014, Montani 2021).
As Olszewski (2014) points out correctly in his article published in the Journal of the History of Medicine and Allied Sciences, statistics are often only a clarifying part of the whole story, and epidemiology can’t always make sense of attributing factors. He suggests using larger epidemiological data supported by longer timelines to observe an effect, which is always the best way forward in interpreting larger-scale phenomena. Moreover, hot debates like the ‘cholesterol myth’ force researchers to become more diligent and aware of possible biases.
LOOKING AT THE BIGGER PICTURE
Where are we today? Decades after Keys was prominently featured on the cover of TIME Magazine, and sometime later his Cholesterol-paradigm was also presented as ‘eggs clogging your arteries’ on another cover of TIME, this ‘promotion’ led to a generalised belief that cholesterol was the ultimate explanation and root cause of cardiovascular incidents. Following this, the demonisation of saturated fats and cholesterol drove the Big Food Industries to switch to hydrogenised vegetable oils, away from (clarified) butter. ‘No Fat’ became the new hype. Consequently, Big Pharma saw a huge opportunity to start working on cholesterol-lowering drugs (statins) as saturated fats, coincidentally, appeared to raise cholesterol levels. Yet, in the last decade, it became clearer that there is little evidence to support this whole thesis (Sinatra et al. 2014), but statins remain the most prescribed drugs on the planet.
Well, today, we are faced with over 41 million preventable deaths from chronic illnesses PER YEAR, in which the majority is attributed to cardiovascular problems. 41% of the global population is overweight, and 15% is obese (Phelps et al. 2024), and cardiovascular disease remains the leading cause of premature deaths worldwide (Braquera et al. 2015), while the trend is still going upwards (Chen et al. 2023).
LET’S UNRAVEL THE CHOLESTEROL MYTH – DOES IT MAKE ANY SENSE?
Cholesterol is a fatty substance used by the body to create cells, support hormone function, produce bile acids, produce Vitamin D, and other substances. Your liver produces 80% of it by itself. So, most likely, the 20% that comes from dietary intake is something we can control fully. The cholesterol group is divided into Low-Density Lipoproteins and High-Density Lipoproteins, in which the latter is considered the ‘GOOD’ cholesterol and is anchored to ApoA, a key to unlock the ‘good’ cholesterol in your system (Hevonoja et al. 2000).
LDL, considered the BAD one, has a function in the body as its particles facilitate cholesterol transport to the liver, from which it is channelled towards cell repair. LDL is aided by Apoliprotein B (ApoB-100), a protein crucial in for LDL transport by removing LDL from the bloodstream into the cells. Consequently, instead of checking your cholesterol levels at large, checking ApoB levels would make more sense (Hevonoja et al. 2000, Welldius et al. 2007). If necessary at all, let’s see.
The traditional optimal values are noted as a maximum of 100mg/dl LDL, and an HDL higher than 60 (Walldius et al. 2007).
Saturated versus Unsaturated Fats
A noticed reduction on saturated fats (SFA) to lower LDL cholesterol blood levels stems from the larger type A, buoyant large particles, while the smaller type B particles are responisive to carb intake and appear responsible for cardiovascular disease (Malhotra 2013), it is also described that saturated fats (SFAs) elevate both LDL AND HDL, a bit at odds with the general believe (Feingold 2012).
If saturated fats are responsible for higher cholesterol levels, why is it that several reviews have found that replacing SFAs with carbs still lead to higher cholesterol levels, while mono- and polyunsaturated fats (MUFA, PUFA) or high-quality carbs all lead to less cardiovascular disease (CVD) (Clifton and Keogh 2017)? A study by Valk et al. (2022) concludes there is no scientific evidence showing a significant association between SFAs and CVD, risks, or events. An analysis of individual-level data in three large cohorts, combined with a meta-analysis, showed opposing dietary correlations in the dietary SFAs, USAFs, and related CVDs; sometimes it shows benefits, in other cases it becomes a risk (Shi et al. 2025). A huge review of 2021 by Lotfi et al. adds more confusion by stating that MUFA is inversely related to a decrease in all-cause mortality, consumption of MUFA was not associated with higher CVDs, cancer, or mortality. This all makes a lot of sense, doesn’t it?!
What can inductive reasoning conclude from all this conflicting information? Other factors could be at play here: ethnicity, race, sex, environment, you name it. But then again, a lot of studies adjust for these variables, and moreover, looking at the global figures, they are on the rise everywhere on the planet. Concurrently, statins are still prescribed ‘en masse’ to lower cholesterol, and still the figures of CVDs keep rising. A lot that does not add up here. Could it be that the SFA/Cholesterol paradigm is just another theory that got out of hand over time by means of so-called ‘consensus’, and was adopted as reality based on nothing more than flawed science from decades ago, followed by more assumptions leading to even more distractions from reality? Could it be that SFAs and cholesterol have little to do at all with CVDs? Let’s dig further…
HDL, remember, the GOOD cholesterol, is supposedly able to decrease LDL. One of the proposed good fatty acids aiding this process is Omega-3. A systematic review and meta-analysis published in Nature concludes that Omega-3-fatty acids reduce cardiovascular mortality and improve outcomes (Khan et al. 2021). In 2023, Von Eckardstein et al. published a scientific paper in the European Heart Journal concluding that excess HDL (above 1,9 mmol/L for men and above 2,4 mmol/L for women) contributes to higher all-cause mortality (see figure 5 by Von Eckardstein et al.).
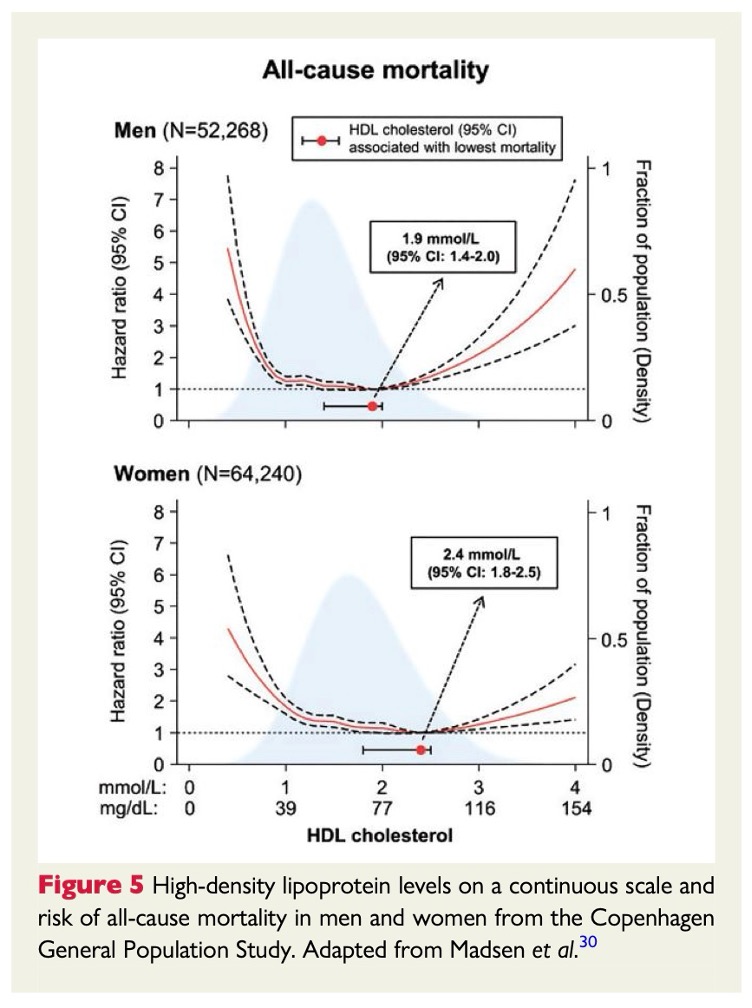
What could we conclude here? Although HDL is proclaimed as the GOOD cholesterol, this research shows clearly that an abundance leads to all-cause excess mortality, so even here we see that the GOOD and BAD cholesterols are relative concepts. Moreover, excess HDL isn’t as harmless as we are meant to believe for overall health.
Some more confusing news, as Casula et al. (2021) found, HDL related to a decrease in atherosclerosis lacks any substantiation, and concludes that randomized control trials do not provide convincing results. Wait, what? So, we have been told for decades that consuming HDL would be protective against developing plaque in the arteries, no? The researchers raise the hypothesis that a variety of physiological functions around cholesterol transport may stem from evolutionary systems. So, it could be merely a genetic difference among mankind?
On the contrary, Lan and Watts (2025) performed a Mendelian (genetic) randomized study demonstrating an increased risk of CVD when HDL particles were larger, conversely, a lower risk when HDL was transported in smaller particles. So, is it genetic predisposition? Or which other variables are at play that we haven’t been taking into account? Or, are they searching in the wrong direction? Anyhow, simply following the HDL discourse does not seem to be the answer to lowering atherosclerosis, as is shown by Kjeldsen et al. (2021), who state that randomised controlled trials aiming to increase HDL uptake failed and only left questions about the role of HDL cholesterol in human health.
STATINS: THE BEST SELLING DRUG FOR LOWERING CHOLESTEROL?
Cochrane, back in the days, the absolute reference when it came to scrutinising evidence, concluded in a major review that statins hardly contributed to the primary prevention of cardiovascular risks and quality of life (Taylor et al. 2011). In 2019, a meta-analysis by Yebyo et al. stated a primary prevention effect in CVD risks; however, they remained unsure of the net cost-benefit of this treatment. In the same year, an overview of systematic reviews by Byrne et al. was published in the British Medical Journal, concluding with mixed findings and widely differing baseline risks. The authors questioned whether statin use justified potential harms. More recently, in 2022, San et al. performed a meta-analysis on statins and stroke prevention; not even a significant correlation was found for mortality or morbidity.
So, what do we know so far? A lower type-A LDL associates with a higher risk for CVDs. Type-B LDL gets triggered by sugar and leads to blood vessel inflammation and plaque. SFAs both raise LDL and HDL, and the latter does not appear to have any effect on better CVD outcomes. Furthermore, statins contribute little to nothing to lowering cholesterol levels. A myriad of non-aligning findings….where is the logic?
When we face a lot of conflicting information, data, and scientific outcomes, we should start to wonder what the reasons may be. Let’s zoom out for a bit. The paradigm started with an assumption supported by questionable evidence. During the 80s, 90s, and 2000s, most studies started their research by assuming a causality between the good and the bad, which in disbalance could lead to plaque in the cardiovascular system, consequently ending in a stroke, heart attack, or heart failure. When you base research on unfounded assumptions, the results can never lead to a well-established finding. What’s more is the fact that many research findings end up with a plethora of diverging outcomes that make it difficult to prove sufficient correlation to assume anything. Could it be that research has been barking up the wrong tree for decades, and that SFAs and LDL are not the root causes for cholesterol? Does cholesterol in itself really form plaques? Until now, we haven’t found any conclusive evidence for any of this.
IS POINTING THE FINGER AT SUGAR SUPPORTED BY EVIDENCE?
Within the last decade, more and more voices have pointed towards sugar as the root cause of atherosclerosis and CVDs, but is it supported by any decent evidence?
A review by DiNicolantonio et al. (2016) looked at the evidence of both the fat-paradigm and studies related to sugar intake leading to coronary heart disease and CVDs. They conclude that more evidence supports the negative impact of sugars as the root cause of chronic heart disease, and they urge a paradigm shift. A way to test if sugars are responsible for CVD is to investigate low-carb diets and cardiovascular risks. Dong et al. (2020) compiled these studies, reviewed them, and performed a meta-analysis of all the results, leading to the conclusion that low-carb diets had a beneficial effect on CVD risks. Could sugar be the trigger? Let’s dig deeper…
As the ketogenic diet gains momentum for several positive outcomes, research in this area may bring more clarity. Keto diets are intrinsically low to very low in carbs. Popiolek-Kalizs (2024) did a review on the topic at hand, which shows that in the short term, the effects of cutting back on carbs are beneficial in lowering blood sugar, body mass, triglycerides, and blood pressure. According to this research, the long-term effects are not yet sufficiently underpinned. A review does give us some broader insights, but does not always allow us to make firm conclusions.
Yin et al. (2021) performed a broad systematic review and meta-analysis where they looked into sugar-sweetened beverages and their outcomes on CVD. They noted a strong dose-dependent association between these drinks and a higher risk of CVD and CDV mortality. Whole foods (complex carbs) and drinks (fast sugars) are hardly comparable as they induce a different metabolic response. Could there be an association between the glycaemic index (GI)/load (GL) and CVDs? Dwivedi et al. (2022) did a follow-up on meta-analysis and cohort studies. They found that GI to enhance risks of CVD and high GL contributes to severe heart disease and all-cause mortality. A study looking into the different types of carbs/sugars and their impact on CVD by Kelly et al. (2023) concluded that non-complex sugars were associated with higher CVD incidence.
Ultra-processed Foods
It becomes apparent that non-complex carbs (sugars and refined starches, as we have plenty of in ultra-processed foods (UPF)) are contributing to higher CVD risk. Specific research on UPF, biomarkers, and CVD risk enlightens a lot. A cohort study of almost 6236 people, of which almost half developed coronary heart disease, and the other half faced an ischemic stroke, was previously followed for almost 25 years. This cohort showed that higher inflammatory and carcinogenic markers, as well as the endothelial cell-specific molecule-1, were positively associated with UPF (Li et al. 2023). Knowing that the inner lining of your arteries consists of these endothelial cells, it may not come as a surprise that low-grade inflammatory responses will lead to plaque and clogging.
Sawalha et al. (2023) state that the long-held belief that lipids form plaque (atherosclerosis) should be revised. Their study on the microbiological pathways explains the impact of sweeteners, sugars, and toxic chemicals in our UPF-chain, resulting in inflammatory chronic diseases, damaging blood vessels, and the disruption of the gut microbiome, enhancing these processes. A cross-sectional study by Ghorbani (2025) comes to the same conclusion.
CONCLUSION
It becomes more and more apparent that the lipid-driven paradigm (SFAs, LDL, HDL, Cholesterol) related to CVDs and mortality is based on many assumptions and flawed research, finding its origins in the past. Still today, we see publications that support this thesis; however, they mostly build upon the assumptions and ‘proofs’ from the past. A self-fulfilling prophecy.
Zooming out, we can only conclude that the massive amount of conflicting evidence and contrasting data presented over the last few decades is inconsistent. This means we have most probably been looking at the wrong root causes all the time. More recent science shows that carbs, and primarily simple sugars, contribute to higher risks of CVD, higher mortality, and comorbidities. But are carbs the only root cause? This remains unclear as studies on ultra-processed foods come to the same conclusion. Within UPFs, sugars and sweeteners are common; however, many other non-whole food substances like chemicals, preservatives, enhancers, and many other non-natural additives are added.
Most probably, the combination of carbs and UPFs, which is part of most people’s dietary regimen today, contributes to the inflammatory processes leading to CVDs, mortality, and comorbidity. More than cholesterol contributes to anything negative. More research is urgently needed to differentiate the impact of UPF ingredients and substances used, to specify and acknowledge the underlying causes for chronic diseases at large. In the meantime, moderate intake of sugars as well as any other UPF is suggested. The only thing we can substantiate with some certainty is that whole foods are the way forward for any human.
REFERENCES
ABOUL-ENEIN, B. H., PUDDY, W. C. & BERNSTEIN, J. 2020. Ancel Benjamin Keys (1904–2004): His early works and the legacy of the modern Mediterranean diet. Journal of Medical Biography, 28, 139-147.
BARQUERA, S., PEDROZA-TOBÍAS, A., MEDINA, C., HERNÁNDEZ-BARRERA, L., BIBBINS-DOMINGO, K., LOZANO, R. & MORAN, A. E. 2015. Global Overview of the Epidemiology of Atherosclerotic Cardiovascular Disease. Archives of Medical Research, 46, 328-338.
CASULA, M., COLPANI, O., XIE, S., CATAPANO, A. L. & BARAGETTI, A. 2021. HDL in atherosclerotic cardiovascular disease: in search of a role. Cells, 10, 1869.
CHEN, W., LI, Z., ZHAO, Y., CHEN, Y. & HUANG, R. 2023. Global and national burden of atherosclerosis from 1990 to 2019: trend analysis based on the Global Burden of Disease Study 2019. Chinese Medical Journal, 136, 2442-2450.
CLIFTON, P. M. & KEOGH, J. B. 2017. A systematic review of the effect of dietary saturated and polyunsaturated fat on heart disease. Nutr Metab Cardiovasc Dis, 27, 1060-1080.
DINICOLANTONIO, J. J., LUCAN, S. C. & O’KEEFE, J. H. 2016. The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease. Progress in Cardiovascular Diseases, 58, 464-472.
DONG, T., GUO, M., ZHANG, P., SUN, G. & CHEN, B. 2020. The effects of low-carbohydrate diets on cardiovascular risk factors: A meta-analysis. PLoS One, 15, e0225348.
DWIVEDI, A. K., DUBEY, P., REDDY, S. Y. & CLEGG, D. J. 2022. Associations of Glycemic Index and Glycemic Load with Cardiovascular Disease: Updated Evidence from Meta-analysis and Cohort Studies. Curr Cardiol Rep, 24, 141-161.
FEINGOLD, K. R. 2021. The effect of diet on cardiovascular disease and lipid and lipoprotein levels.
GHORBANI, Z., DASHTI, F., GRAFENAUER, S., ARAMI, S., MAHDAVI-ROSHAN, M. & SALARI, A. 2025. Ultra-processed foods and coronary artery disease severity: a cross-sectional study of at-risk normal-weight and overweight patients undergoing elective angiography. J Health Popul Nutr, 44, 63.
HEVONOJA, T., PENTIKÄINEN, M. O., HYVÖNEN, M. T., KOVANEN, P. T. & ALA-KORPELA, M. 2000. Structure of low-density lipoprotein (LDL) particles: basis for understanding molecular changes in modified LDL. Biochimica et Biophysica Acta (BBA)-Molecular and cell biology of lipids, 1488, 189-210.
KELLY, R. K., TONG, T. Y. N., WATLING, C. Z., REYNOLDS, A., PIERNAS, C., SCHMIDT, J. A., PAPIER, K., CARTER, J. L., KEY, T. J. & PEREZ-CORNAGO, A. 2023. Associations between types and sources of dietary carbohydrates and cardiovascular disease risk: a prospective cohort study of UK Biobank participants. BMC Med, 21, 34.
KHAN, S. U., LONE, A. N., KHAN, M. S., VIRANI, S. S., BLUMENTHAL, R. S., NASIR, K., MILLER, M., MICHOS, E. D., BALLANTYNE, C. M. & BODEN, W. E. 2021. Effect of omega-3 fatty acids on cardiovascular outcomes: a systematic review and meta-analysis. EClinicalMedicine, 38.
KJELDSEN, E. W., NORDESTGAARD, L. T. & FRIKKE-SCHMIDT, R. 2021. HDL Cholesterol and Non-Cardiovascular Disease: A Narrative Review. Int J Mol Sci, 22.
LAN, N. S. R. & WATTS, G. F. 2025. New perspectives on the high-density lipoprotein system and its role in the prevention and treatment of atherosclerotic cardiovascular disease. Current Opinion in Endocrinology, Diabetes and Obesity, 32, 66-74.
LI, H., WANG, Y., SONESTEDT, E. & BORNÉ, Y. 2023. Associations of ultra-processed food consumption, circulating protein biomarkers, and risk of cardiovascular disease. BMC Medicine, 21, 415.
LOTFI, K., SALARI-MOGHADDAM, A., YOUSEFINIA, M., LARIJANI, B. & ESMAILLZADEH, A. 2021. Dietary intakes of monounsaturated fatty acids and risk of mortality from all causes, cardiovascular disease and cancer: A systematic review and dose-response meta-analysis of prospective cohort studies. Ageing Research Reviews, 72, 101467.
MALHOTRA, A. 2013. Saturated fat is not the major issue. BMJ : British Medical Journal, 347, f6340.
MONTANI, J. P. 2021. Ancel Keys: The legacy of a giant in physiology, nutrition, and public health. Obesity Reviews, 22, e13196.
OLSZEWSKI, T. M. 2014. The Causal Conundrum: The Diet-Heart Debates and the Management of Uncertainty in American Medicine. Journal of the History of Medicine and Allied Sciences, 70, 218-249.
PHELPS, N. H., SINGLETON, R. K., ZHOU, B., HEAP, R. A., MISHRA, A., BENNETT, J. E., PACIOREK, C. J., LHOSTE, V. P. F., CARRILLO-LARCO, R. M., STEVENS, G. A., RODRIGUEZ-MARTINEZ, A., BIXBY, H., BENTHAM, J., DI CESARE, M., DANAEI, G., RAYNER, A. W., BARRADAS-PIRES, A., COWAN, M. J., SAVIN, S., RILEY, L. M., AGUILAR-SALINAS, C. A., BAKER, J. L., BARKAT, A., BHUTTA, Z. A., BRANCA, F., CAIXETA, R. B., CUSCHIERI, S., FARZADFAR, F., GANAPATHY, S., IKEDA, N., IOTOVA, V., KENGNE, A. P., KHANG, Y.-H., LAXMAIAH, A., LIN, H.-H., MA, J., MBANYA, J. C. N., MIRANDA, J. J., PRADEEPA, R., RODRÍGUEZ-ARTALEJO, F., SORIĆ, M., TURLEY, M., WANG, L., WEBSTER-KERR, K., AARESTRUP, J., ABARCA-GÓMEZ, L., ABBASI-KANGEVARI, M., ABDEEN, Z. A., ABDRAKHMANOVA, S., ABDUL GHAFFAR, S., ABDUL RAHIM, H. F., ABDURRAHMONOVA, Z., ABU-RMEILEH, N. M., ABUBAKAR GARBA, J., ACOSTA-CAZARES, B., ADAM, I., ADAMCZYK, M., ADAMS, R. J., ADU-AFARWUAH, S., AEKPLAKORN, W., AFSANA, K., AFZAL, S., AGBOR, V. N., AGDEPPA, I. A., AGHAZADEH-ATTARI, J., ÅGREN, Å., AGUENAOU, H., AGYEMANG, C., AHMAD, M. H., AHMAD, N. A., AHMADI, A., AHMADI, N., AHMADI, N., AHMED, I., AHMED, S. H., AHRENS, W., AITMURZAEVA, G., AJLOUNI, K., AL-HAZZAA, H. M., AL-HINAI, H., AL-LAHOU, B., AL-LAWATI, J. A., AL-RADDADI, R., AL ASFOOR, D., AL HOURANI, H. M., AL QAOUD, N. M., ALAROUJ, M., ALBUHAIRAN, F., ALDHUKAIR, S., ALDWAIRJI, M. A., ALEXIUS, S., ALI, M. M., ALIEVA, A. V., ALKANDARI, A., ALKERWI, A. A., ALKHATIB, B. M., ALLIN, K., ALOMARY, S. A., ALOMIRAH, H. F., ALSHANGITI, A. M., et al. 2024. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. The Lancet, 403, 1027-1050.
POPIOLEK-KALISZ, J. 2024. Ketogenic diet and cardiovascular risk – state of the art review. Current Problems in Cardiology, 49, 102402.
SAN, X., LV, Z., XU, P., WANG, J. & LAN, T. 2022. The prevention of stroke by statins: A meta-analysis. Medicine (Baltimore), 101, e30606.
SAWALHA, K., TRIPATHI, V., ALKHATIB, D., ALALAWI, L., MAHMOOD, A. & ALEXANDER, T. 2023. Our Hidden Enemy: Ultra-Processed Foods, Inflammation, and the Battle for Heart Health. Cureus, 15, e47484.
SHI, F., CHOWDHURY, R., SOFIANOPOULOU, E., KOULMAN, A., SUN, L., STEUR, M., ALEKSANDROVA, K., DAHM, C. C., SCHULZE, M. B. & VAN DER SCHOUW, Y. T. 2025. Association of circulating fatty acids with cardiovascular disease risk: analysis of individual-level data in three large prospective cohorts and updated meta-analysis. European journal of preventive cardiology, 32, 233-246.
SINATRA, S. T., TETER, B. B., BOWDEN, J., HOUSTON, M. C. & MARTINEZ-GONZALEZ, M. A. 2014. The saturated fat, cholesterol, and statin controversy a commentary. Journal of the American College of Nutrition, 33, 79-88.
TAYLOR, F., WARD, K., MOORE, T. H., BURKE, M., DAVEY SMITH, G., CASAS, J. P. & EBRAHIM, S. 2011. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev, Cd004816.
VALK, R., HAMMILL, J. & GRIP, J. 2022. Saturated fat: villain and bogeyman in the development of cardiovascular disease? European journal of preventive cardiology, 29, 2312-2321.
WALLDIUS, G. & JUNGNER, I. 2007. Apolipoprotein A-I versus HDL cholesterol in the prediction of risk for myocardial infarction and stroke. Curr Opin Cardiol, 22, 359-67.
YEBYO, H. G., ASCHMANN, H. E., KAUFMANN, M. & PUHAN, M. A. 2019. Comparative effectiveness and safety of statins as a class and of specific statins for primary prevention of cardiovascular disease: A systematic review, meta-analysis, and network meta-analysis of randomized trials with 94,283 participants. American Heart Journal, 210, 18-28.
YIN, J., ZHU, Y., MALIK, V., LI, X., PENG, X., ZHANG, F. F., SHAN, Z. & LIU, L. 2021. Intake of Sugar-Sweetened and Low-Calorie Sweetened Beverages and Risk of Cardiovascular Disease: A Meta-Analysis and Systematic Review. Advances in Nutrition, 12, 89-101.
Disclaimer
The views and analysis expressed in this content (video, blog, article, etc.) are solely that of the author and does not necessarily reflect the views of humani-well, the organisation, or other associated parties.
Medical disclaimer: you should not rely on the information on this website as a replacement for seeing a doctor or other qualified healthcare provider for a diagnosis or treatment. Nothing in this publication should be interpreted as a substitute for the advice of a qualified healthcare provider. Please consult a medical professional before using any information contained in this publication.
Drs. Sam Brokken
Next to guiding this bunch of great people at Humani-Well, Sam covers a broad range of topics. From biomedical issues to societal impact analysis. HIs biggest strength? Being a 'generalist, and master of none'. Know More
© 2025 Humaniwell | CHOOSE WISELY. Powered by NoCodeLabs.